The skincare market is a multi-billion dollar industry, one in which people throughout the world spend billions of dollars on skin-care products each year in the hopes that it will help keep their skin looking young and healthy. Aging skin is a common concern and the skin-care market has been growing steadily for years. Global sales are projected to reach $183 billion by 2025, according to an analysis by Report Buyer, a marketing research company.
There may not be a magic formula to turn back the clock on our skin, but some products, in addition to a healthy lifestyle, may help delay some of these inevitable changes in the skin’s appearance, like fine lines and wrinkles. These fine creases, along with other signs of aging like dryness and age spots, have one major common cause — exposure to ultraviolet light.
Aging is a part of the growing process, and there is no set way to look younger than you are, but there are ways to help slow the pace. Sleeping well, eating healthy foods, and exercising may all seem impossible in today’s busy environment but they are all important in how your body ages.
To identify what happens to your skin as it ages, 24/7 Tempo reviewed several clinical studies and research published in the International Dermal Institute and various journals such as Aging Cell. Unfortunately, how you treat your body may show on your skin — and these are 20 bad and common habits that are aging people really fast.
Here is what happens to your skin as you age
1. It loses elasticity

As people get older, the dermis, which is the thicker and deeper layer of the skin, can lose from 20% to 80% of its thickness due to changes in the cells responsible for collagen and elastin biosynthesis. These proteins are produced at a slower rate, affecting the skin’s structure, and causing it to hang loosely and become slack. Changes in elastin fibers are typical in elderly people, sometimes leading to a condition called elastosis. In solar elastosis, caused by sun damage, the skin looks yellow and can develop bumps.
2. It takes longer to heal

Eccrine sweat glands, which secrete sweat to the skin surface to help cool a person’s body temperature, also help heal wounds. These glans are a source of new cells that replace the ones lost to injury. However, this process does not work as well in older adults as it does in younger people, according to research published in Aging Cell. There are fewer new cells available to heal wounds, and they are located farther apart, resulting in a delayed healing process. The reason is not that the glands were less active, but that the degraded aging skin was less able to support the new cells.
3. It develops benign tumors

A benign tumor is a non-malignant growth of cells, which means it does not spread. Benign tumors have been linked to ultraviolet radiation coming from the sun. Skin tags and moles are examples of benign tumors, and aging skin is more prone to developing them. Medically, they are a benign proliferation of melanocytes, which are the cells that produce the protective skin-darkening pigment melanin.
4. It becomes transparent

It is not uncommon for the skin to become more transparent in elderly people, especially in those with rheumatoid disease. Veins on the hands, wrists, ribs, and shins of elderly people can be seen through the skin. Clinical studies of biopsies found that collagen fibers, which are what keep the skin firm and looking young, are not as closely packed in transparent skin as they are in more opaque skin.
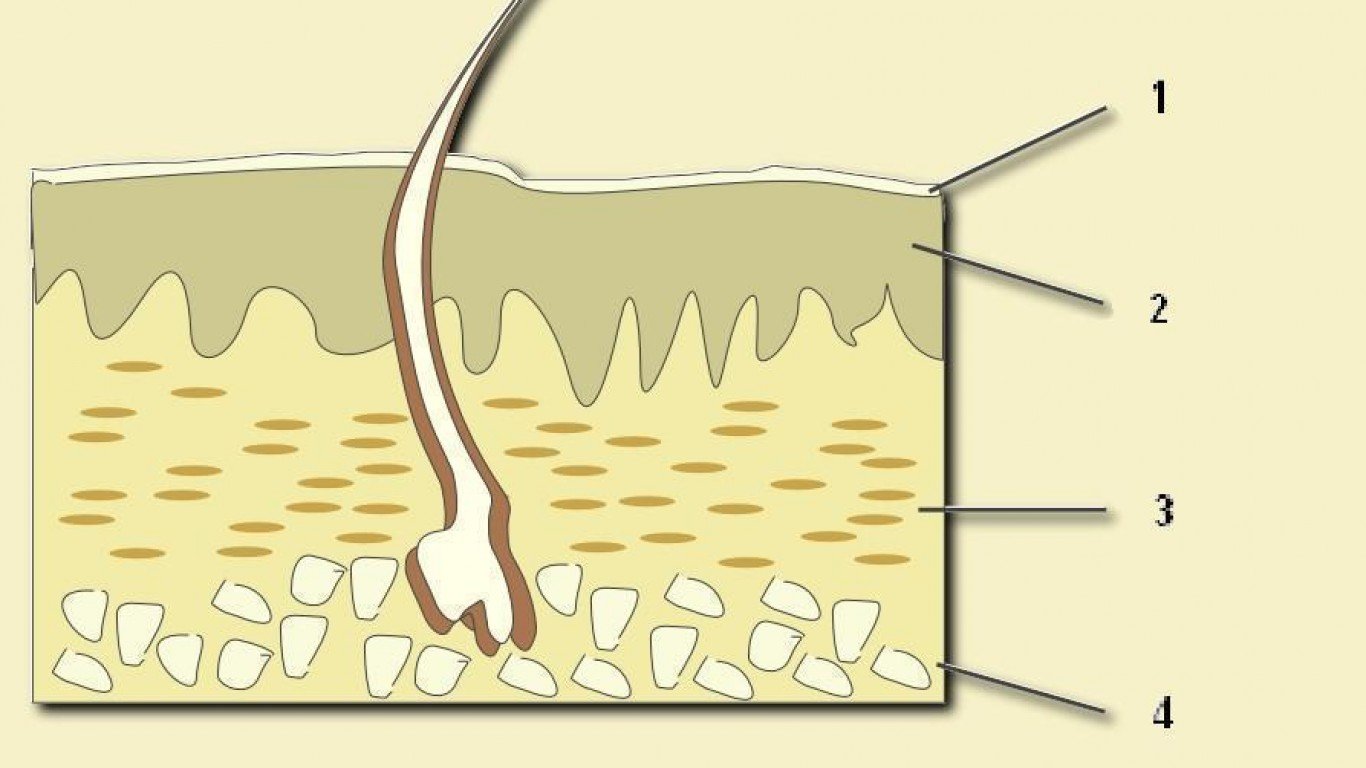
5. It loses a protective layer of fat
The inner layer of the dermis, or subcutaneous layer, is where the sweat glands, some hair follicles, blood vessels, and fat are found in the skin. As we age, this protective layer of fat thins, providing less insulation to the skin and making it more fragile and susceptible to injury. Older people may therefore be more sensitive to cold, heat, and touch.
6. It bruises easily

Bruising is common in older adults because the skin is thinner. Due to the loss of some of the fat that protects the blood vessels from injuries, blood vessels can break more easily with blood leaking out, forming a bruise.
7. It becomes rough, dry, and itchy

Sebaceous glands are responsible for lubricating the skin and will produce less oil with age. This is visible mostly in older women, whose glands gradually start making less oil after menopause. The lower levels of sebum, the oily matter secreted by the gland, mean lower levels of moisture in the skin, which can cause dryness and itchiness.
8. It retains more heat

Sweat glands become less efficient over time which is why older people sweat less than younger adults. These glands produce less sweat, which makes controlling body temperature more difficult. The risk of overheating and heat strokes increases with age.
9. It grows cherry bumps

Cherry angiomas, also known as cherry bumps, look like little red moles and are a result of an overgrowth of capillaries. Most common among people older than 30, these dilated blood vessels often appear on the chest, stomach, or back. Why exactly they develop is not clear, but they are not a cause of concern unless they bleed often or change color or size.
10. It becomes less responsive to some meds

The innermost layer of the skin consists of fat and connective tissue. Because it contains many blood vessels and nerves, it easily absorbs medications. Some medications, such as those for acne and dermatitis, are absorbed by the fat layer that the skin thins out as people age. Hence, the meds are less effective.
11. It can become very dry

The medical term for dry skin is xerosis and while it can affect anyone, it is more common among older people. As the skin ages, it loses water and oils, making it more difficult to retain moisture. The skin gets dry and appears rough and hardened.
12. Epidermis becomes thinner

As people get older, the skin becomes thinner gradually – at an average rate of about 6.4% per decade, according to research. While age does not lower the number of skin cell layers, it affects their strength. The epidermis, the outer layer of the skin, decreases in thickness, particularly in the face, neck, upper part of the chest and hands, and the back of forearms.
13. Age spots appear

Age spots – small, dark brown areas on the skin that, unlike freckles, don’t fade — can technically appear on all skin types but are more common in older people with light skin. The most common parts of the body where they appear are in parts exposed to the sun, such as shoulders, hands, face, and arms. Age spots are not a health problem unless they change in appearance, which may be a sign of skin cancer.
14. Blood vessels become fragile

As you age, blood vessels lose elasticity, which makes them more susceptible to breaking. Common conditions associated with fragile blood vessels of the dermis are bruising, bleeding under the skin, and cherry angiomas (red moles on the skin). The most common parts of the body where bruising can occur as a result of this are the back of the arms and legs.
15. Pressure ulcers
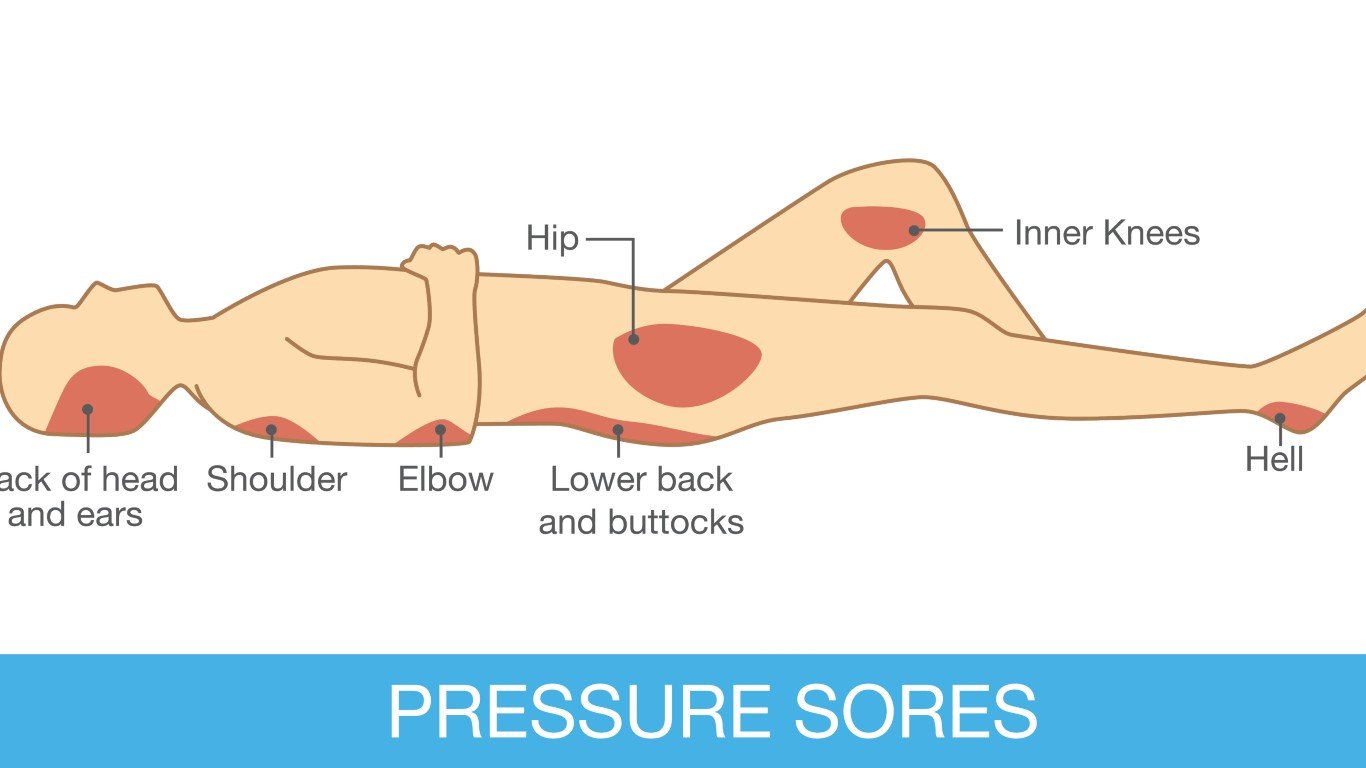
Pressure ulcers are often referred to as bed sores, implying that only people who are bed-bound develop them. While reduced mobility is a major risk factor for pressure ulcers, people who can walk can also get pressure ulcers. Skin changes, including the loss of fat layers in the dermis, can cause pressure ulcers, according to the National Institutes of Health. The skin’s slower healing process as a result of aging can contribute to sores and other skin infections as well.