There were more than 24 million overnight hospital stays in the United States in 2017 alone. While the likelihood of a full and speedy recovery following treatment varies depending on the nature of the illness or condition, other factors, including the quality of medical care, can play a significant role.
There are over 6,200 hospitals in the United States, and not all of them are equally effective. While it is difficult to precisely determine the quality of a specific health care system, there are certain measures that can be indicative of overall quality of care.
24/7 Wall St. created an index of three such measures at the metro area level to identify the cities with the worst health care system outcomes.
The first measure we included in our index is the metro area level hospital readmission rate — or the share of Medicare patients readmitted to the hospital within 30 days of initial discharge. The second index component is the hospital mortality rate — or the share of Medicare patients who die within 30 days of admittance to a hospital. The third and final measure is the rate of preventable hospitalizations — or the frequency at which Medicare patients are admitted to a hospital for conditions that could or should have been treated in an outpatient setting.
In an interview with 24/7 Wall St., Matthew Fiedler, a fellow with USC-Brookings Schaeffer Initiative for Health Policy, explained that while these measures can be useful in determining the quality of care for a given hospital or health care system, they can also be the product of other factors unrelated to the quality of care.
“Variation across areas does seem to reflect differences in how well the health system is working,” Fiedler said. “But you also have to be very cautious.”
How good the hospital is at delivering care and ensuring appropriate follow-up after the patient is discharged is only one broad set of factors that can influence the measures used to create this list. “And the other broad bucket of factors is what types of patients is the hospital treating,” Fiedler said.
Indeed, the socioeconomic characteristics of a metro area population do appear to have an impact on the measures used to rate health care system performance, including those related to personal health. For example, unhealthy patient behaviors like smoking, sedentary lifestyles, and poor diets, can contribute to higher readmission rates and higher mortality rates. In fact, based on measures such as these, many of the cities on this list have relatively unhealthy populations. Here is a look at the least healthy city in each state.
It is also likely no coincidence that in the majority of metro areas on this list, most households have far lower incomes than the typical American household. “I think there are certainly mechanisms […] that would cause less advantaged areas to have less effective health care systems,” Fiedler said. These include hospital facilities having fewer resources and an insufficient number of doctors in an area.
Many of the cities on this list rank among the poorest nationwide. Here is a closer look at the 50 poorest metro areas in the United States.

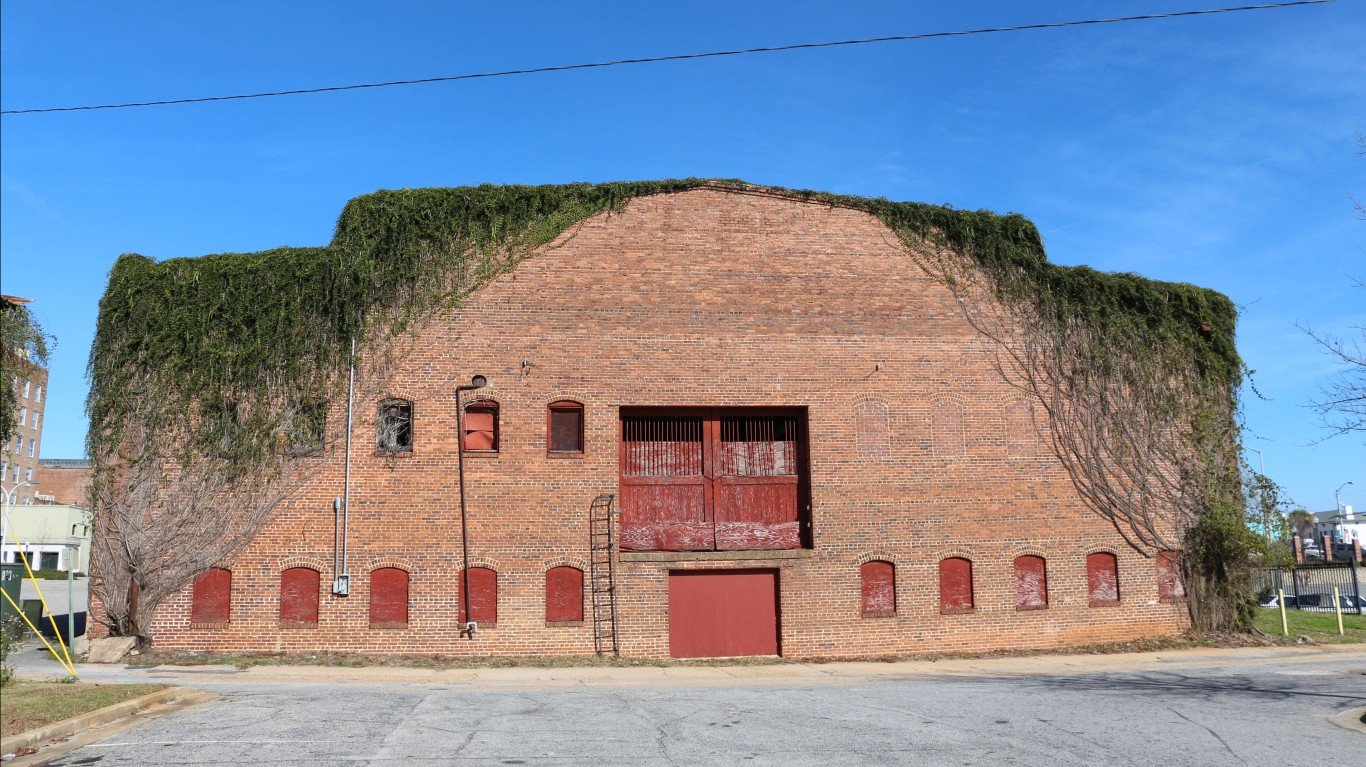
25. Mobile, AL
> 30-day hospital readmission rate: 15.6%
> Mortality within 30 days of hospitalization: 13.2%
> Preventable hospitalizations: 60.7 per 1,000 Medicare enrollees
> No. of physicians: 65.6 per 100,000
> Median household income: $43,061
There are only about 66 primary care physicians for every 100,000 people in Mobile, Alabama, lower than the national concentration of 75 per 100,000. An inadequate number of doctors in a city can make it more difficult to seek necessary preventive and primary care, which can lead to an overreliance on hospitals. And in Mobile, a larger than typical share of residents are hospitalized for conditions that could or should have been treated in an outpatient setting. There are about 61 preventable hospitalizations for every 1,000 Medicare enrollees in the metro area, compared to 45 per 1,000 nationwide.
As is the case in most metro areas on this list, Mobile residents are more likely to be disadvantaged economically than the typical American. The median annual household income in Mobile is $43,061, well below the national median of $61,937.

24. Beckley, WV
> 30-day hospital readmission rate: 15.7%
> Mortality within 30 days of hospitalization: 12.5%
> Preventable hospitalizations: 69.6 per 1,000 Medicare enrollees
> No. of physicians: 74.4 per 100,000
> Median household income: $38,917
One of the main indicators of hospital quality is the share of patients being readmitted after discharge. Readmissions can occur due to poor post-acute care, medical complications during initial hospital stays, poor patient discharge instructions, or for other, non-preventable medical reasons. In Beckley, 17.0% of all heart attack patients are readmitted to the hospital after 30 days, the 12th largest share of any U.S. metro area. Additionally, 24.3% of patients with heart failure return to the hospital within 30 days of discharge, the eighth largest share.
Another measure of health care quality is the number of patients hospitalized for conditions that are treatable in an outpatient setting — often an indication of poor outpatient treatment. In Beckley, there are 70 preventable hospitalizations per 1,000 Medicare enrollees, the ninth highest ratio in the country.
23. Goldsboro, NC
> 30-day hospital readmission rate: 15.7%
> Mortality within 30 days of hospitalization: 14.3%
> Preventable hospitalizations: 47.6 per 1,000 Medicare enrollees
> No. of physicians: 51.6 per 100,000
> Median household income: $40,791
Along with Burlington and Rocky Mount, Goldsboro is one of three North Carolina metro areas to rank on this list. In Goldsboro, some 14.3% of patents die within 30 days of being admitted to a hospital’s care, one of the highest rates of any metro area and well above the corresponding 12.4% national rate.
Wealthier Americans are better equipped to afford regular, preventative health care and can afford a greater range of healthy options related to diet and lifestyle — and as a result, income is closely linked to health outcomes. As is the case in most metro areas on this list, Goldsboro residents are more likely to be disadvantaged economically than the typical American. The median annual household income in Goldsboro is just $40,791, over $20,000 below the national median of $61,937.

22. Gulfport-Biloxi, MS
> 30-day hospital readmission rate: 15.9%
> Mortality within 30 days of hospitalization: 13.1%
> Preventable hospitalizations: 59.5 per 1,000 Medicare enrollees
> No. of physicians: 50.9 per 100,000
> Median household income: $47,444
There are just 51 primary care physicians per 100,000 residents in the Gulfport-Biloxi metro area, far less than the national concentration of 75 physicians per 100,000 Americans. With less access to outpatient treatment, Gulfport residents may be more likely to visit the hospital for conditions that are treatable in a primary care setting, putting themselves at unnecessary risk of infection or increased frailty from inactivity during their hospital stay. There are 60 such preventable hospitalizations in Gulfport per 1,000 Medicare enrollees, among the most of any U.S. metro area.
Poorer areas often have worse healthcare systems than wealthier areas. In Gulfport, the typical household has an income of $47,444 a year, approximately $14,500 less than the U.S. median.

21. Burlington, NC
> 30-day hospital readmission rate: 15.0%
> Mortality within 30 days of hospitalization: 15.4%
> Preventable hospitalizations: 44.9 per 1,000 Medicare enrollees
> No. of physicians: 47.0 per 100,000
> Median household income: $49,979
Burlington, North Carolina, has the second highest post-hospitalization mortality rate of any metro area in the United States. Some 15.4% of patients die within 30 days of being admitted to the hospital, the second largest share of any U.S. metro area and well above the national rate of 12.4%.
The high post-hospitalization mortality rate may be attributable in part to the insufficient number of available doctors in Burlington. There are just 47 primary care physicians for every 100,000 metro area residents, a smaller concentration than in the vast majority of metro areas. For context, there are 75 primary care physicians per 100,000 people nationwide.

20. Hanford-Corcoran, CA
> 30-day hospital readmission rate: 16.1%
> Mortality within 30 days of hospitalization: 13.4%
> Preventable hospitalizations: 53.3 per 1,000 Medicare enrollees
> No. of physicians: 39.4 per 100,000
> Median household income: $61,663
There are just 39 primary care physicians per 100,000 residents in the Hanford-Corcoran metro area, the 12th least of any metro area nationwide. A low doctor-to-population ratio can contribute to preventable hospitalization — with less access to outpatient services, residents may be more likely to visit the hospital for primary care-sensitive conditions, putting themselves at increased risk of infection or increased frailty from inactivity. There are 53 preventable hospitalizations per 1,000 Medicare enrollees in Hartford, eight more than the corresponding U.S. average.
Another possible indication of a poorly functioning healthcare system is the percentage of patients who return to the hospital within a month of discharge. In Hanford, 16.1% of patients return to the hospital within 30 days of discharge, among the most of any U.S. metro area.
19. Longview, TX
> 30-day hospital readmission rate: 17.5%
> Mortality within 30 days of hospitalization: 12.0%
> Preventable hospitalizations: 50.2 per 1,000 Medicare enrollees
> No. of physicians: 56.6 per 100,000
> Median household income: $51,296
In Longview, Texas, those who are hospitalized are more likely to be readmitted within a month of discharge than those in every other U.S. metro area. Though unplanned readmissions are usually not the hospital’s fault, they can also be caused by such avoidable conditions as a surgical wound infection. In Longview, 17.5% of people discharged from hospitals are readmitted within 30 days, well above the 15.3% readmission rate nationwide.
Preventable hospitalizations are also more common in Longview than they are nationwide. An overreliance on hospital care can be indicative of insufficient outpatient treatment, and in Longview, access to outpatient care may be limited by the availability of doctors. There are only about 57 primary care physicians for every 100,000 people, substantially lower than the national ratio of 75 per 100,000.

18. Monroe, MI
> 30-day hospital readmission rate: 16.5%
> Mortality within 30 days of hospitalization: 12.5%
> Preventable hospitalizations: 59.1 per 1,000 Medicare enrollees
> No. of physicians: 31.5 per 100,000
> Median household income: $61,916
One factor affecting the quality of health care in Monroe may be the relative lack of doctors in the metro area. There are just 31 primary care physicians per 100,000 residents in Monroe, less than half the national concentration of 75 doctors per 100,000 Americans. With less access to outpatient treatment, Monroe residents may be more likely to visit the hospital for primary care-sensitive conditions, putting unnecessary strain on hospital resources.
Monroe is the only metro area in Michigan, and one of only three metro areas in the Midwest, to rank on this list.

17. Port St. Lucie, FL
> 30-day hospital readmission rate: 16.8%
> Mortality within 30 days of hospitalization: 12.4%
> Preventable hospitalizations: 56.8 per 1,000 Medicare enrollees
> No. of physicians: 46.6 per 100,000
> Median household income: $55,714
In Port St. Lucie, Florida, 16.8% of patients are hospitalized again within 30 days of their discharge. High 30-day readmission rates can sometimes be indicative of lower quality care in area hospitals, and only six other metro areas nationwide have a higher readmission rate than Port St. Lucie.
The area’s poor performance in measures of quality of care may be partially due to an overreliance on hospitals as a primary treatment option. There are about 57 hospitalizations for conditions that should have been treated in an outpatient setting for every 1,000 Medicare enrollees in Port St. Lucie, a higher share than in the vast majority of U.S. metro areas and well above the national preventable hospitalization rate of 45 per 1,000.

16. Johnstown, PA
> 30-day hospital readmission rate: 16.3%
> Mortality within 30 days of hospitalization: 13.3%
> Preventable hospitalizations: 52.7 per 1,000 Medicare enrollees
> No. of physicians: 82.4 per 100,000
> Median household income: $45,084
Poorer areas tend to have underperforming hospital systems and worse health care overall. In Johnstown, the typical household has an income of just $45,084 a year, nearly $17,000 less than the U.S. median.
One possible indication of poor hospital quality is high patient readmission. While readmissions are often no fault of the hospital, readmissions can occur due to poor post-acute care, medical complications during initial hospital stays, or inadequate patient discharge instructions. In Johnstown, 17.2% of all heart attack patients return to the hospital within 30 days of discharge, the third highest share of any metro area.

15. Ocala, FL
> 30-day hospital readmission rate: 15.4%
> Mortality within 30 days of hospitalization: 15.3%
> Preventable hospitalizations: 44.3 per 1,000 Medicare enrollees
> No. of physicians: 58.7 per 100,000
> Median household income: $44,576
Along with Lakeland and Port St. Lucie, Ocala is one of three Florida metro areas to rank on this list. Ocala’s ranking is primarily attributable to the high post-hospitalization mortality rate in the area. Some 15.3% of those admitted to area hospitals die within 30 days — either in the hospital or after returning home — the fourth highest share of metro areas nationwide. Death rates for those hospitalized with pneumonia is particularly high, at 21.5%, well above the corresponding 15.6% national rate.
Post-hospitalization mortality rates are not necessarily attributable to hospital errors. Often, they are the result of unhealthy patient behaviors — and certain unhealthy behaviors are slightly more common in Ocala. Adults in Ocala are more likely to smoke and be obese and less likely to exercise than the typical American adult.

14. Bowling Green, KY
> 30-day hospital readmission rate: 16.4%
> Mortality within 30 days of hospitalization: 12.9%
> Preventable hospitalizations: 58.6 per 1,000 Medicare enrollees
> No. of physicians: 55.5 per 100,000
> Median household income: $51,365
There are just 56 primary care physicians per 100,000 residents in Bowling Green, far less than the national corresponding ratio of 75 per 100,000. A low doctor-to-resident ratio may result in a high number of patients visiting hospitals for conditions that are treatable in outpatient settings. Such preventable hospitalizations can increase the risk of infection and frailty due to hospital stays, and can be an indication of poor access to outpatient care. In Bowling Green, there are 59 preventable hospitalizations per 1,000 Medicare enrollees, among the most of any U.S. metro area.
Another possible indication of health care quality is the number of patients who return to the hospital after being discharged, which can sometimes be due to medical complications incurred while in treatment. Some 16.4% of patients in Bowling Green return to the hospital within 30 days of discharge, the 17th highest share of any U.S. metro area.
13. Albany, GA
> 30-day hospital readmission rate: 16.1%
> Mortality within 30 days of hospitalization: 13.9%
> Preventable hospitalizations: 51.3 per 1,000 Medicare enrollees
> No. of physicians: 67.0 per 100,000
> Median household income: $44,896
In Albany, Georgia, 13.9% of hospital patients die within 30 days of admission to the hospital. While this can be indicative of poor quality hospital care, it can also be attributable to the patient’s own behaviors and health — and many in Albany have unhealthy habits. For example, smoking is the leading cause of preventable death in the United States, and in Albany, more than 20% of adults smoke, well above the 17.0% national smoking rate.
Some other measures, however, also suggest the possibility of below-average quality of care in Albany hospitals. For example, 16.1% of those discharged from area hospitals are readmitted within 30 days, a higher share than the 15.3% national readmission rate. Unplanned hospital readmissions are often the result of preventable errors, like infections of surgical wounds.
12. Carbondale-Marion, IL
> 30-day hospital readmission rate: 17.1%
> Mortality within 30 days of hospitalization: 12.8%
> Preventable hospitalizations: 51.1 per 1,000 Medicare enrollees
> No. of physicians: 106.0 per 100,000
> Median household income: $42,716
In the Carbondale-Marion metro area, 17.1% of patients return to the hospital within 30 days of being discharged, the fifth largest share of any metro area. While the majority of hospital readmissions are non-preventable, many are due to poor post-acute care or medical complications incurred during initial treatment.
One of the largest determinants of the quality of a local health system is income. Wealthier areas are often more likely to attract qualified health professionals and have more resources to fund hospitals and outpatient treatment centers. In Carbondale, the typical household has an income of just $42,716 a year, over $19,000 less than the U.S. median and the 18th lowest of any metro area nationwide.

11. Dubuque, IA
> 30-day hospital readmission rate: 15.0%
> Mortality within 30 days of hospitalization: 12.7%
> Preventable hospitalizations: 83.3 per 1,000 Medicare enrollees
> No. of physicians: 75.3 per 100,000
> Median household income: $60,225
Dubuque, Iowa, is one of only three metro areas in the Midwest to rank on this list. Preventable hospitalizations can suggest inadequate outpatient treatment and also a tendency to overuse hospitals as a primary source of care. In Dubuque, about 83 Medicare enrollees for every 1,000 are hospitalized for conditions that could or should have been treated in an outpatient setting, the largest share of any metro area in the United States.
Despite the nation-leading preventable hospitalization rate and the unnecessary additional strain that such hospitalizations imposes on area facilities, by some measures, hospitals in Dubuque perform relatively well. For example, just 15.0% of those discharged by area hospitals are readmitted within 30 days, a smaller share than the 15.3% national readmission rate.

10. Parkersburg-Vienna, WV
> 30-day hospital readmission rate: 16.5%
> Mortality within 30 days of hospitalization: 13.1%
> Preventable hospitalizations: 56.9 per 1,000 Medicare enrollees
> No. of physicians: 76.5 per 100,000
> Median household income: $44,054
Poorer areas tend to have underperforming hospital systems and worse health care overall. In the Parkersburg-Vienna metro area, the typical household earns just $44,054 a year, nearly $18,000 less than the U.S. median.
One indication of poor hospital quality can be high patient readmission. While the majority of hospital readmissions are non-preventable, many are due to poor post-acute care or medical complications incurred during initial treatment. In Parkersburg, 16.5% of all patients return to the hospital within 30 days of discharge, the 12th largest share of any U.S. metro area.

9. Jackson, TN
> 30-day hospital readmission rate: 15.6%
> Mortality within 30 days of hospitalization: 14.8%
> Preventable hospitalizations: 54.5 per 1,000 Medicare enrollees
> No. of physicians: 105.0 per 100,000
> Median household income: $45,610
The rate of patients dying within 30 days of being admitted to a hospital in Jackson, Tennessee, is nearly the highest of any city in the United States. Some 14.8% of patients discharged from metro area hospitals die within 30 days, a higher share than in all but 11 other U.S. metro areas. The 30-day mortality rate for patients treated for pneumonia is particularly high — 20.1% compared to 15.6% nationwide.
Wealthier Americans are better equipped to afford regular, preventative health care and healthier options related to diet and lifestyle — and as a result, income is closely linked to health outcomes. As is the case in nearly every other metro area in this list, Jackson residents are more likely to be disadvantaged economically than the typical American. The median annual household income in Jackson is $45,610, well below the $61,937 national median.
8. Pine Bluff, AR
> 30-day hospital readmission rate: 16.7%
> Mortality within 30 days of hospitalization: 14.3%
> Preventable hospitalizations: 47.5 per 1,000 Medicare enrollees
> No. of physicians: 51.1 per 100,000
> Median household income: $37,314
Adjusted for risk factors such as age, patient health, and the presence of other chronic diseases, residents of Pine Bluff are more likely to die after receiving treatment in area hospitals than in a majority of metro areas. Some 14.3% of patients treated for conditions including heart attack, COPD, heart failure, pneumonia, and stroke die within 30 days of being admitted to the hospital, a larger share than the 12.4% comparable national mortality rate.
Pine Bluff residents are also among the most likely in the nation to have to return to the hospital after receiving care. Some 16.7% of patients in Pine Bluff are readmitted to the hospital within 30 days of discharge, the eighth largest share nationwide. While the majority of hospital readmissions are non-preventable, many are due to medical complications incurred during initial treatment or poor post-acute care.

7. Hattiesburg, MS
> 30-day hospital readmission rate: 16.4%
> Mortality within 30 days of hospitalization: 13.3%
> Preventable hospitalizations: 64.8 per 1,000 Medicare enrollees
> No. of physicians: 84.5 per 100,000
> Median household income: $45,249
High unplanned hospital readmission rates are a burden on the health care system, costing Medicare an estimated $17 billion annually. High readmission rates can also sometimes be indicative of low-quality care. In Hattiesburg, Mississippi, 16.4% of people discharged from the hospital are readmitted within 30 days, higher than the 15.3% national readmission rate.
Poor quality care in Hattiesburg could be partially due to area hospitals being spread thin. For every 1,000 Medicare enrollees, there are about 65 preventable hospitalizations, well above the corresponding rate of 45 per 1,000 nationwide. Hospitalizations for conditions that could or should have been treated in an outpatient setting suggest an overreliance on hospitals and an inefficient distribution of resources.

6. Vineland-Bridgeton, NJ
> 30-day hospital readmission rate: 17.1%
> Mortality within 30 days of hospitalization: 12.5%
> Preventable hospitalizations: 74.7 per 1,000 Medicare enrollees
> No. of physicians: 42.9 per 100,000
> Median household income: $52,795
There are just 43 primary care physicians per 100,000 residents in the Vineland-Bridgeton metro area, one of the lowest concentrations of any city in the country. With fewer doctors per capita, Vineland residents may be more likely to go to the hospital for conditions that are treatable in a primary care setting, exposing themselves to risk of infection during their hospital stay and adding unnecessary strain on hospital resources. There are 75 such preventable hospitalizations in Gulfport per 1,000 Medicare enrollees, the fourth highest rate of any U.S. metro area.
Another possible indication of poor quality of care is a higher share of patients who return to the hospital within a short period after discharge, often due to infection or other medical complications incurred during treatment. Some 17.1% of patients in Vineland return to the hospital within 30 days of discharge, the fourth largest share among U.S. metropolitan areas.

5. Lakeland-Winter Haven, FL
> 30-day hospital readmission rate: 16.6%
> Mortality within 30 days of hospitalization: 13.4%
> Preventable hospitalizations: 69.6 per 1,000 Medicare enrollees
> No. of physicians: 49.2 per 100,000
> Median household income: $51,670
For every 1,000 people enrolled in Medicare in the Lakeland metro area, there are about 70 hospitalizations for conditions that could or should have been treated in an outpatient facility. This suggests a possible overreliance on hospitals in the metro area and also potentially a lower than typical quality of care in some outpatient facilities in the metro area.
Also, in Lakeland, those who are hospitalized are more likely to be readmitted within a month of discharge than those discharged from hospitals in the vast majority of other metro areas nationwide. Though unplanned readmissions are not always the fault of the hospital, they can be caused by such conditions as a surgical wound infection. In Lakeland, 16.6% of people discharged from hospitals are readmitted within 30 days, the 10th highest share among U.S. metro areas.

4. Wheeling, WV-OH
> 30-day hospital readmission rate: 15.8%
> Mortality within 30 days of hospitalization: 14.4%
> Preventable hospitalizations: 72.5 per 1,000 Medicare enrollees
> No. of physicians: 80.4 per 100,000
> Median household income: $49,749
Wheeling is one of many poor metro areas in which the incidence of hospital readmission, post-treatment mortality, and preventable hospitalization is worse than the nation as a whole. The typical household in Wheeling has an annual income of just $49,749, over $12,000 less than the U.S. median.
Adjusted for risk factors such as age, patient health, and the presence of other illnesses, patients in Wheeling are more likely than the average patient to die within a month after being admitted to a hospital. Some 15.3% of heart attack patients die within 30 days of being admitted to the hospital, the seventh largest share of any U.S. metro. Some 19.6% of pneumonia patients and 5.2% of coronary artery bypass patients die within 30 days, the seventh and fifth largest shares, respectively.

3. Merced, CA
> 30-day hospital readmission rate: 17.5%
> Mortality within 30 days of hospitalization: 14.3%
> Preventable hospitalizations: 52.5 per 1,000 Medicare enrollees
> No. of physicians: 44.7 per 100,000
> Median household income: $57,745
In the Merced, California, metro area, 17.5% of all hospital patients who are discharged are readmitted within 30 days, the third largest share of any metro area in the United States. Though the majority of unplanned hospital readmissions are not preventable, an especially high readmission rate can be indicative of poor quality hospital care.
Adequate physician availability is critical to receiving necessary care, and there are relatively few doctors in the Merced metro area. There are only about 45 primary care physicians for every 100,000 people in Merced, one of the smallest shares among U.S. metro areas and well below the national concentration of 75 per 100,000.

2. Rocky Mount, NC
> 30-day hospital readmission rate: 16.2%
> Mortality within 30 days of hospitalization: 14.9%
> Preventable hospitalizations: 67.8 per 1,000 Medicare enrollees
> No. of physicians: 47.5 per 100,000
> Median household income: $46,733
Adjusted for risk factors such as age, patient health, and the presence of other illnesses, those recently hospitalized in Rocky Mount are more likely to die — either in the hospital or at home — than patients in almost any other city. Some 14.9% of Rocky Mount residents being treated for conditions like COPD, heart failure, heart attack, pneumonia, and stroke die within 30 days of being admitted to the hospital, the 11th largest share of any U.S. metro area.
Rocky Mount residents are also relatively likely to be admitted to the hospital for conditions that could be treated in an outpatient setting, putting unnecessary strain on hospital resources and exposing themselves to increased risk of infection and other medical complications due to hospital stays. There are 68 preventable hospitalizations per 1,000 Medicare enrollees in Rocky Mount, far more than the national rate of 45 preventable hospitalizations per 1,000 Medicare enrollees nationwide.

1. Jonesboro, AR
> 30-day hospital readmission rate: 17.1%
> Mortality within 30 days of hospitalization: 13.8%
> Preventable hospitalizations: 68.2 per 1,000 Medicare enrollees
> No. of physicians: 98.6 per 100,000
> Median household income: $43,927
Preventable hospitalizations — or hospitalizations for illnessnesses and conditions that could or should have been treated in an outpatient setting — are an unnecessary strain on hospital resources. In Jonesboro, Arkansas, there are 68 preventable hospitalizations per 1,000 Medicare enrollees, more than in all but 11 other metro areas nationwide. For context, the national preventable hospitalization rate is 45 per 1,000.
The added strain may be impacting the quality of care in the metro area. Hospital readmission rates are one of the most commonly cited measures of the quality of a region’s health care system, and readmissions are relatively common in Jonesboro. Some 17.1% of discharged patients are readmitted to the hospital within 30 days of their initial treatment, a larger share than in all but five other U.S. cities and well over the 15.3% national rate.
Methodology
To determine the cities where you don’t want to get sick, 24/7 Wall St. created an index using data for U.S. metropolitan statistical areas from the Centers for Medicare and Medicaid Services (CMS) and County Health Rankings. The index measures three sets of indicators: 30-day mortality rates, 30-day readmission rates, and preventable hospitalizations. Mortality and readmission rates each make up 42.1% of the index, and the rate of preventable hospitalizations makes up the remaining 15.8%.
The CMS produces statistics on numerous health measures for more than 4,000 Medicare-certified hospitals in the country. We grouped hospitals by metropolitan areas and aggregated the hospital data to the metropolitan statistical area level.
Mortality rates
We calculated a weighted average of 30-day mortality rates for heart attacks, chronic obstructive pulmonary disease (COPD), coronary artery bypass grafting (CABG), heart failure, pneumonia, and stroke patients to find the average percentage of people who died within 30 days of being admitted to a hospital. The mortality measures are adjusted for differences in risk variables such as age, comorbidities — the presence of multiple ailments for a given patient — and patient frailty. CMS estimates the data for 30-day mortality by each condition per hospital from Medicare patients.
Readmission rates
The readmission rate measures are estimates of unplanned readmission to an acute care hospital in the 30 days after discharge from a hospital for Medicare beneficiaries 65 or older. Patients may have an unplanned readmission for any reason.
Preventable hospitalization
Lastly, we used the share of hospitalizations for conditions that could have been treated at outpatient or ambulatory care facilities — often referred to as the preventable hospitalization rate. This measure counts hospitalizations for conditions such as asthma, dehydration, or hypertension per 1,000 Medicare enrollees. This data is from the 2019 County Health Rankings report, an annual analysis produced by the Robert Wood Johnson Foundation and University of Wisconsin Population Health Institute joint program.
Data on income are one-year estimates from the U.S. Census Bureau’s 2018 American Community Survey. Population figures are from the Census Bureau’s Population Projections program and are estimates for July 2018. Data on the share of residents living in urban and rural areas are from the Census Bureau’s 2010 decennial census.
Measures of individual health behaviors and outcomes including obesity, smoking rates, and sedentary lifestyles also came from County Health Rankings.